In the beginning,
Late last year I was doing some gardening on the top section of our yard, the landscape is split level, meaning the right side of my body was on the downslope. In digging out the base of a small tree stump, I grabbed the final piece with both hands and yanked it out of the ground, unfortunately, it was during this motion that I immediately felt a burst of pain in the right hip and knee.
Fast forward to the 1st of March, for the previous 3 months I had been seeing an Orthopedic Surgeon to discuss options regarding my hip (as I have a labrum tear) but I also wanted to discuss my knee as this started to cause some issues – let’s get a scan! is always the answer.
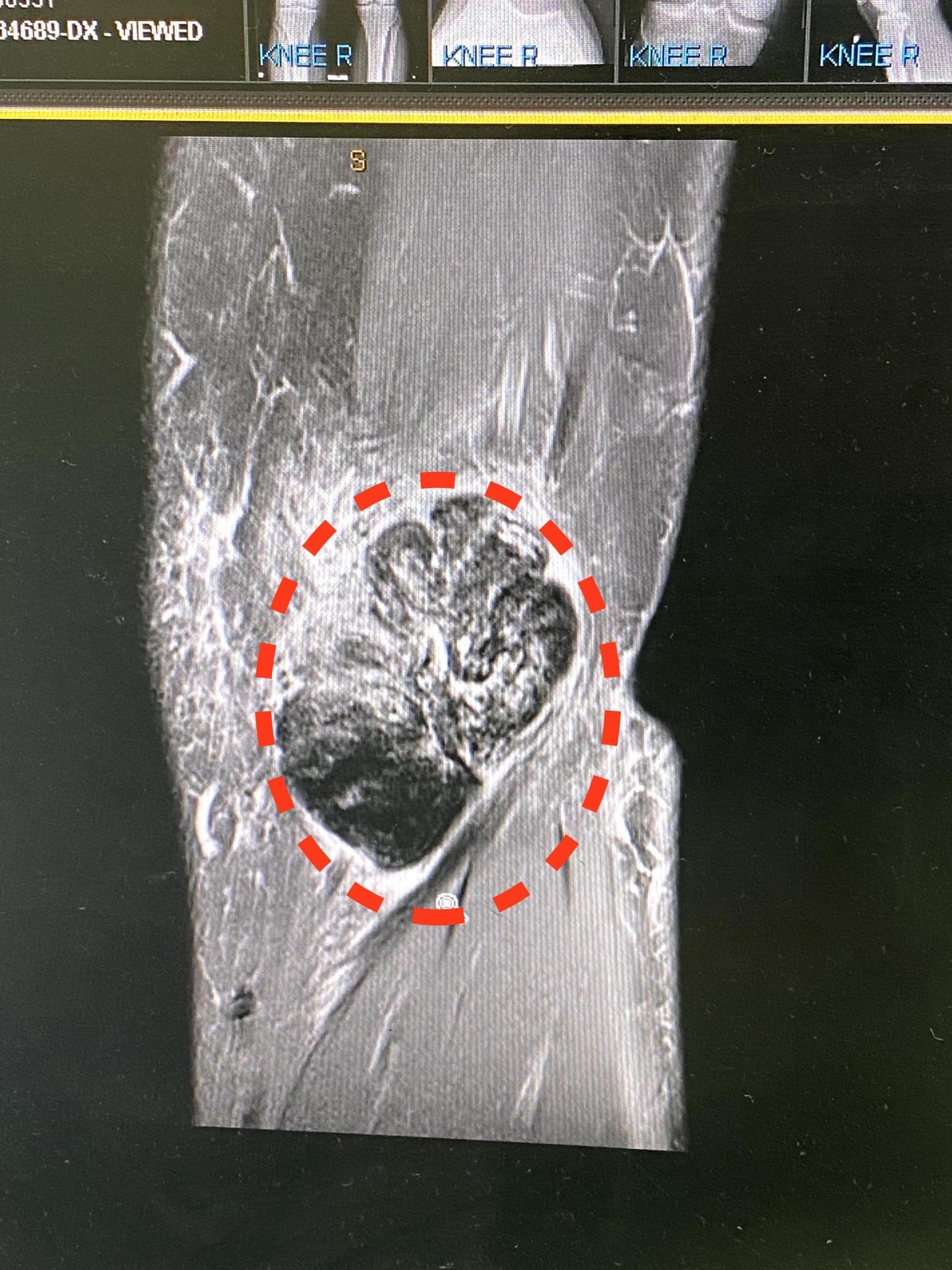
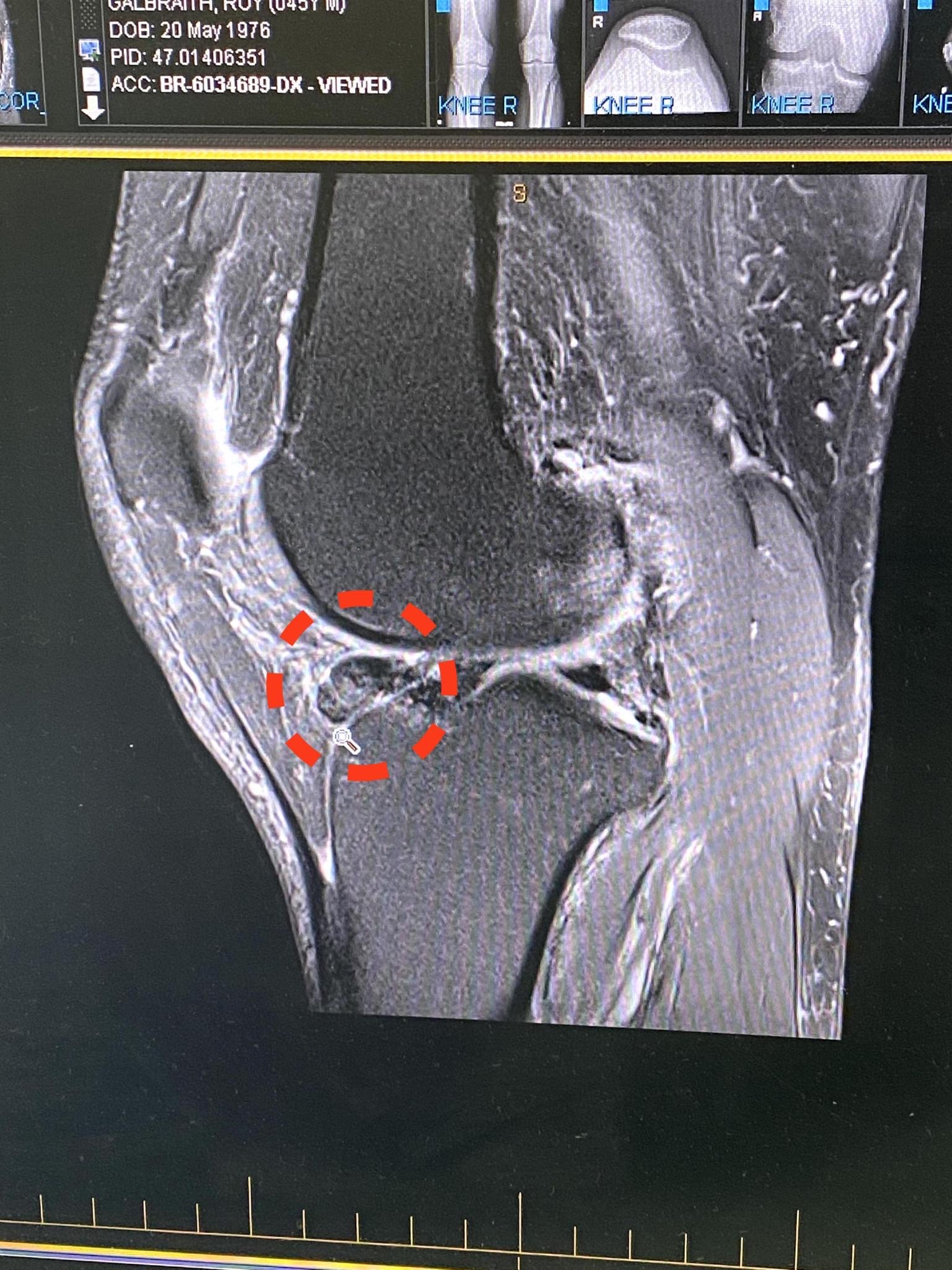
1st March – sitting in the waiting room thinking about what the scan may or may not have shown, Roy, yes that’s me. As we entered the clinical room a little small talk was made, how has the knee been? etc nothing more to see really, then Dr C explains what the scan revealed – looks like you have a torn meniscus and we would treat that with an arthroscopy, but what we need to discuss is the following – it appears that you have 2 tumours in and around the knee. Was that a train that just hit me in the face, are you serious, the mind then buzzes – for those that know, this is not the first time I have heard that word “Tumour”… and I tell you it doesn’t get better the more times you hear it.
So many questions and so few answers, but when you hear the word Tumour your mind plays tricks and it is then very hard to completely take everything else in terms of what is being said, the next keywords were – “I will be referring you to the Tumour Clinic at Flinders Cancer Clinic” for further care/treatment. Hey, this is not my first rodeo, can we have a quick chat about options, I was not looking for a clinical plan in terms of treatment. I wanted to understand deeper what it was and from an orthopedic viewpoint only how this would be tackled. Surgically remove the tumour on the inside of the knee, arthroscopically repair the tear but the concern was the tumour is basically right in the middle of the knee joint between the Femur and the Tibia, there was further chat about whether the tumour is attached to the bone or not.
As I was on my own, it was certainly news that I had to share with my beautiful wife but this comes with its own set of challenges, questions that you don’t have answers to, potential flashbacks, the waiting game and then the next decision – who do you tell and what do you say, the reality is the journey is just beginning and you often don’t have the answers. As we didn’t have any answers we kept the information pretty much to ourselves until we knew what we were dealing with, but even this has its challenges, in that each family member needs their own outlet.
4th April – A month has passed, and in the driver’s seat, no one experiences this more than the patient and the immediate family, the waiting game, not knowing as once you know you can then work towards the resolution. The reason for the delay consisted of a couple of moments, the first being a small admin issue with the referral not arriving in the right location but once it had been received my “case” was triaged and the decision was made to send me for more scans to get a complete picture.
Today (04/04) was the answer day, let’s not beat around the bush… the diagnosis was better than we had planned for 100%, it is a rare disorder called Pigmented Villonodular Synovitis (PVNS), it is thought to affect 2 people in every 1 million. While the initial diagnosis was a huge win and relief, this disorder comes with its own sets of challenges, the particular tumour name is Giant Cell Tumour.
What is it?
GCT – is a rare, aggressive non-cancerous tumour.
Can it be cancerous?
Quote “never say never” but in very rare circumstances, every tumour is sent for lab testing
How is it treated?
Surgery (it must be removed)
Can it reoccur?
Yes, it is an aggressive tumour and is poorly understood, there is no scientific evidence to suggest it is passed on in families or certain activities but does have a 40% recurrence rate even with complete removal.
What is the recovery time?
2 weeks at home rest (forgot to ask about sports etc)
Is it painful?
Well I am not going to lie, it’s shit and it is painful 24×7, activity definitely makes it worse, but so does sitting in a chair for long periods of time and when you are in bed, the pain doesn’t go away – the trick is medication, this doesn’t remove the pain completely but allows you to manage.
What does this mean for me?
Back to my story, we have been advised that while I have 2 well-formed tumours (as below), there are approx 2-3 pebbles within and around the joint to consider as well, these must be removed. If untreated the risk is the tumour keeps growing, but will bleed, this will then have further impacts and will attack the bone and cartilage causing more damage.
What’s Next?
It’s all about timing really, and we need to digest the information and listen to our options, at the end of the day we listen and make a decision. We have agreed to have a review in 8 weeks and during this time I am required to keep a pain diary so the medical team can accurately define a way forward in terms of surgery. The challenge is the tumour that is in the knee joint itself, how they can actually get to that part of the knee while keeping as much of your own body intact is what the consideration is. I could opt for a complete knee replacement but this would be going against the advice of the experts, although this is a real possibility.

Wow Roy, so sorry to read this and hear of your struggles
My thoughts and well wishes
are with you and the family!
Such a stressful and challenging time for you all
Wishing a successful outcome and speedy recovery
Xxx Tanya
LikeLiked by 1 person